| Name: |
|
|
Classification:
|
- Opiate, Narcotic analgesic
|
|
Mechanism of Action:
|
- Binds with opioid receptors. Blocks response to and perception of pain
- Causes histamine induced peripheral venous vasodilatation (decreases SVR)
|
|
Indications:
|
- Moderate to severe pain relief
- AMI/ACS
- CHF
|
|
Contraindications:
|
- Known hypersensitivity
- Hypotension (beware of low SBP in head injured patients)
- Renal failure (relative contraindication due to neurotoxic metabolites, experts generally prefer other opioids such as fentanyl or hydromorphone as first-line however evidence shows that if the dose is appropriately reduced, morphine can be safe)
|
|
Precautions:
|
- Use with caution in the elderly, asthma, and those who may already have or be susceptible to CNS depression
- Use with caution if right ventricular infarct is suspected
- Fast administration is more often associated with adverse effects listed below and can also potentiate a local rash at the IV site. Such local reaction shouldn’t be interpreted as allergy as this is a known effect.
- Opioids should always be used with caution and in reduced dose in older adults or patients with dementia due to the potential for drug accumulation and increased sensitivity to CNS active medications.
- Dose reduction is also required if comorbidities such as COPD, sleep apnea, obesity or any other condition which may increase risk of sedation or cardiorespiratory depression.
- Dose reduction is required for opioid naïve patients.
|
|
Adverse Effects:
|
- Respiratory depression
- Hypotension
- Palpitations
- Dry mouth
- Bradycardia
- Tachycardia
- Constricted pupils
- Altered mental status
- Headache
- Nausea and vomiting
|
|
Dose:
|
|
|
Adult:
|
- 2 - 5 mg IV q 5 - 10 minutes prn; max 20 mg
- 5 - 10 mg IM
|
|
Pediatric:
|
- 0.1 mg/kg IV max per dose 2.5 mg q 5 - 10 minutes prn
- 0.1 mg/kg IM max 5 mg per dose
|
| Routes: |
|
| Special Notes: |
- IN fentanyl is preferred for the pediatric population.
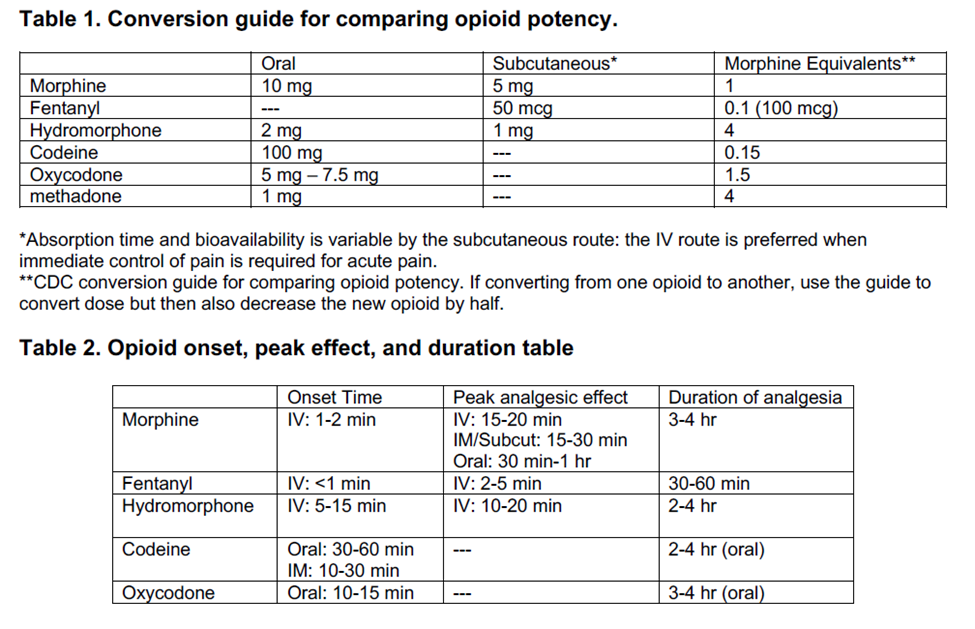
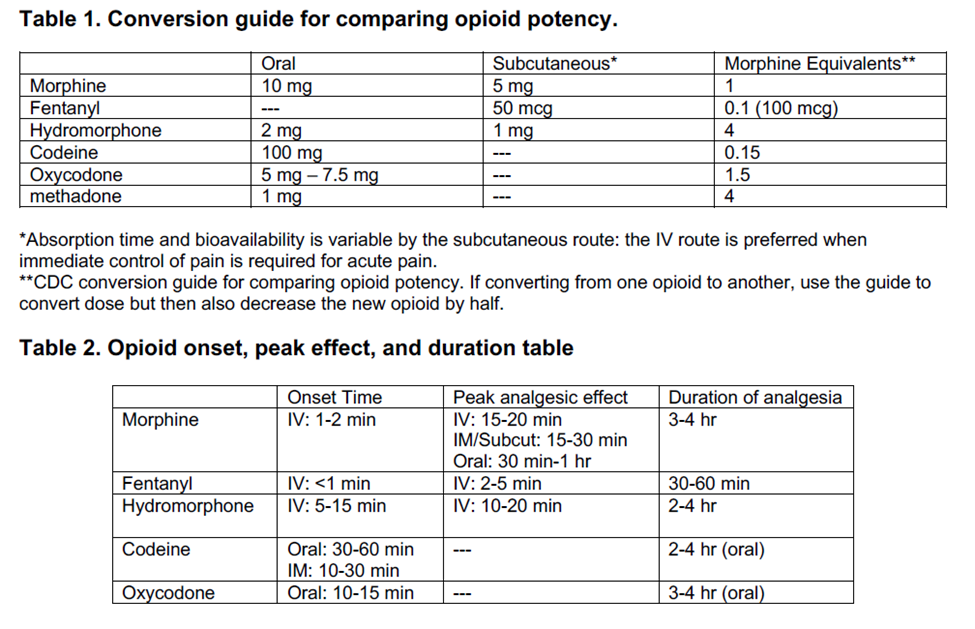
- Morphine lasts approximately 3-6 hours regardless of route. The subcutaneous route is reserved for palliative patients at end stage or patients where an IV is unobtainable. The subcut route has significant disadvantage of variable absorption. For acute pain careful IV titration of morphine or fentanyl is preferred as the absorption is predictable and rapid thereby leading to more rapid pain relief in a safer manner than the subcut route. For palliative patients who are actively dying and unable to take oral medication, the subcut route is preferred as its less painful than starting an IV. For palliative patients in acute pain who would still accept IVs within their goals of care, their pain should be managed via IV route.
- The effects of opioids can be accentuated by CNS depressants such as benzodiazepines, alcohol, or other sedating medications/drugs.
- Opioids should not be combined with benzodiazepines unless for the purpose of procedural sedation. In such circumstances, greatly reduced doses should be used as the sedating and respiratory depressant effects of each are exacerbated by the other. The Clinical Support Paramedic must be contacted prior to giving opioids in conjunction with benzodiazepines to the same patient. If considering procedural sedation, fentanyl is preferred due to its shorter duration of action.
- Fentanyl is preferred for the management of ischemic chest pain unresponsive to nitrates due to its decreased effects on hemodynamic stability.
- The Centers for Disease Control and Prevention (CDC) recommends non-opioid pain relievers such anti-inflammatories and acetaminophen be used as adjuncts to help reduce the amount of opioid required and thereby minimize their associated risks. Using non-opioid pain relievers such as ketorolac or acetaminophen and non-pharmacological techniques are important adjuncts which can be helpful in minimizing the amount of opioid required.
- Fentanyl is the preferred agent to use for the management of pain during labour due to its shorter duration of action.
- Pregnancy category C [if the patient will benefit from a Category C drug, it is generally used]
|
| References: |
- Compendium of Pharmaceuticals and Specialties (CPS)
- Pharmacology for the Prehospital Provider 2nd Edition
|
Last modified: Wednesday, 26 March 2025, 3:28 PM